DEFINING CONCUSSIONS
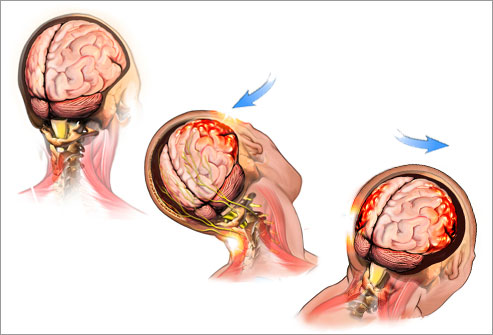
Concussions are a form of mild brain trauma that result in temporary disruption of normal neurological functioning. Concussions are caused by a bump, blow or jolt to the head or by a hit to the body that causes the head and brain to move or stop abruptly. This sudden movement causes the brain to shift and contact the inside of the skull causing physiological changes to the affected neurons.
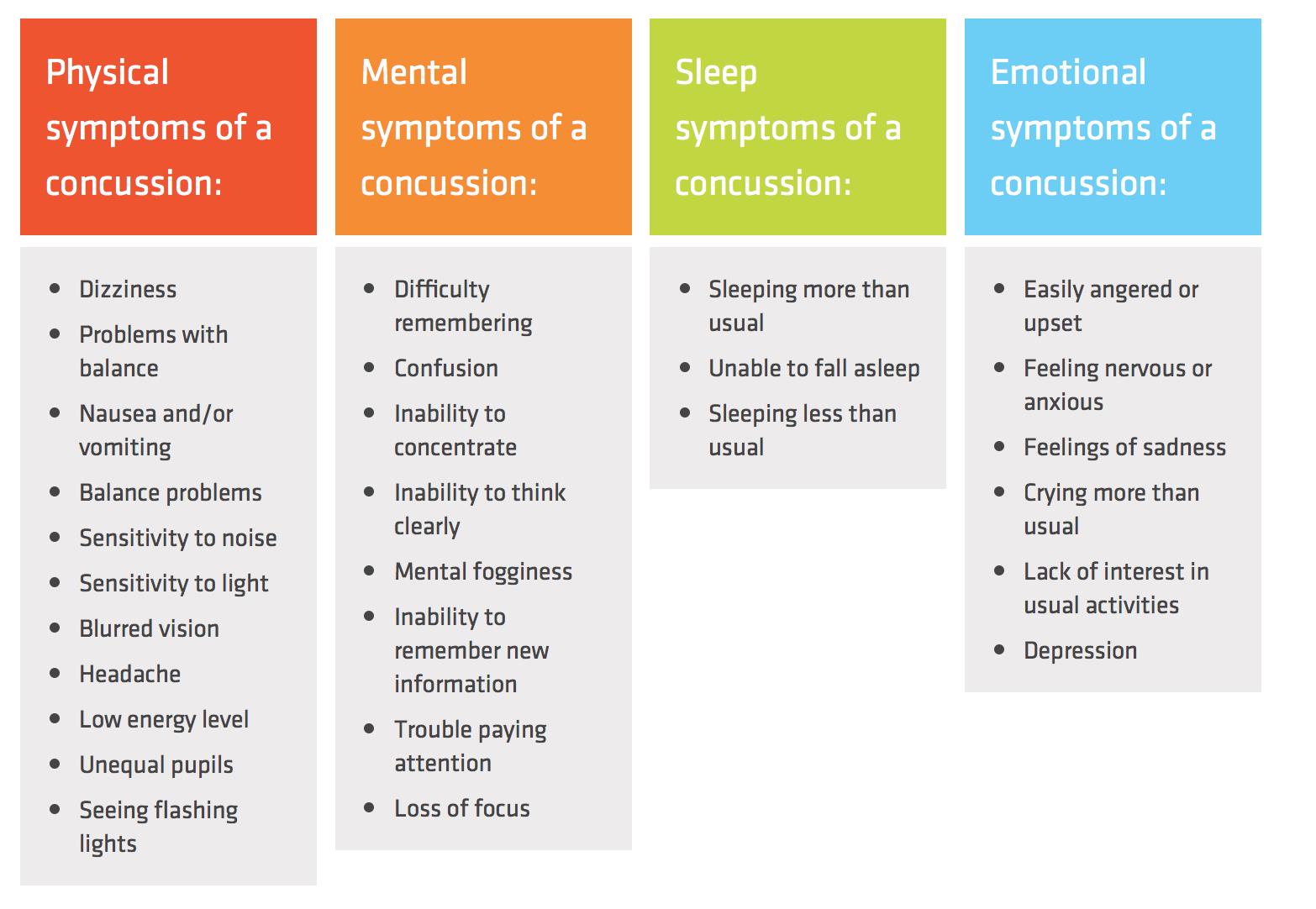
SYMPTOMS OF A CONCUSSION
Important Notes:
- Concussions do not require a loss of consciousness. In fact, approximately 90% of concussions are not accompanied with a loss of consciousness.
- The appearance of concussion signs or symptoms may be delayed several hours or even days following the original mechanism. It is important to continue to monitor someone who has suffered a head injury for several days before completely ruling out a concussion.
- If a student-athlete complains of any of the above symptoms after sustaining a blow to the head or body as described above it is important to immediately notify the school's athletic trainer to allow them to evaluate the injury and determine if it is indeed a concussion. Disclosure of these symptoms and any resulting head injury to the school's athletic trainer is required by school policy.
Finally, nearly all documented cases of Second Impact Syndrome have involved adolescent-aged athletes. Second Impact Syndrome is a catastrophic event resulting from a subsequent concussive episode prior to the brain fully recovering from a previous concussion. This subsequent concussive injury sets off a cascade of events leading to rapidly-escalating metabolic crisis and massive brain swelling that often can lead to death. No other age group has been determined to be at risk for Second Impact Syndrome.
TREATING CONCUSSIONS
When signs or symptoms of a concussion arise during athletic participation the first step is to immediately remove the student-athlete from participation. Research has shown that athletes who are not removed immediately after a concussive injury are approximately 9 times more likely to experience a prolonged recovery. Additionally, athlete who were not removed needed nearly twice as long to recover and experienced more severe post-injury symptoms than those who were removed immediately.
The second step is to report the injury to the school's athletic trainer. The school's athletic trainer can then assess the student-athlete and determine whether a concussion has been sustained and the best course of action. If the injury occurs outside of a school sport or during a time when the athletic trainer is unavailable, you can contact your primary-care physician or local concussion specialist (see below) for further evaluation, or seek care at your local hospital's Emergency Department if any of the following red-flag symptoms present.
Head Injury Red Flags
- Loss or decreased level of consciousness during or after injury
- Severely worsening headache
- Seizures
- Unequal pupil size
- Slurred or incomprehensible speech
- Repetitive vomiting
- Increased confusion
- Unusual behavioral changes or increased irritability/combativeness
- Weakness, numbness, tingling, or paralysis in arm(s) or leg(s)
These red flag symptoms may be a sign of a more significant brain trauma, such as an intracranial hemorrhage, which can be life threatening. However, in the absence of these red flag symptoms, it is not necessary to seek immediate emergency intervention or advanced imaging for a sports-related concussion. Conventional CT and MRI scans are most often found to be normal in sports-related concussions and only expose the patient to high levels of unnecessary radiation.
If the student-athlete is evaluated by a qualified health-care provider (i.e., MD, DO, NP, PA, or athletic trainer per the State of Michigan) and has been diagnosed with a concussion or is being monitored for a concussion, the following are best practice recommendations.
| It is OK to: | There is NO need to: | Do NOT: | |
| Use Acetaminophen (Tylenol) 24 hours after injury | Attend school - Keeping in mind school may trigger additional symptoms | Check eyes with a flashlight | Take Ibuprofen, Aspirin, Naproxen or other NSAID medications unless directed by physician |
| Use an ice pack on head/neck area as needed | Begin light activity (i.e., walking, stationary biking) as symptoms allow after 24-hours post-injury | Wake up every hour | Drive with visual symptoms or severe symptoms |
| Return to activity classes when cleared to do so; notify teachers/counselors of concussion | Take breaks if symptoms increase | Avoid all stimulation; Stay in dark quiet room | Take long or repetitive naps during the day |
| Stick to your normal sleep schedule and eat a normal healthy diet | Allow symptoms to dictate your exertion | Stay in bed | Participate in strenuous activities or sports; push through activities that increase symptoms |
MHSAA CONCUSSION RULES
The MHSAA requires that any student-athlete who exhibits signs or reports symptoms of a concussion resulting from participation in a sport be removed from participation until they are evaluated and cleared by a qualified provider (i.e., MD, DO, NP, PA). This clearance must be written and unconditional and be completed on the MHSAA Return to Activity form, which also requires parent and student consent. This clearance must be obtained before the student-athlete may return to full and/or contact practice or contests.
ZEELAND HIGH SCHOOLS CONCUSSION POLICY
Zeeland East and West High Schools have adopted a stricter concussion policy in order to adhere to evidence-based, best practice standards for concussion management. This policy is in addition to the MHSAA rules and is required for any student-athlete to return to sport after a concussion.
Zeeland Concussion Policy Outlined
- Disclosure of any head or brain injury and/or signs or symptoms to the school athletic trainer
- Disclosure of any diagnosed concussion(s), regardless of origin, to school athletic trainer
- Compliance with school-adopted Return to Activity Protocol (RTAP) prior to clearance
- Acknowledgment that school athletic trainer will have final decision in student-athlete's return to participation regardless of outside provider recommendations or clearance.
Recovery and Return to Play
Because the human brain is so unique from individual to individual, there is no 'one size fits all' approach for concussion management or return to play timeline. Instead, each concussion management plan should be individualized based on physical and neurocognitive findings, preexisting health history, and other contributing factors.
Early Activity and Return to Play Process
Recent research has shown evidence that light, aerobic activity early in the recovery process (but not before 24-hours post-injury) can increase the brain's natural healing factors, causing overall recovery time to decrease. Biking, walking, body weight and balance exercises can be utilized in this early phase but should be discontinued if symptoms increase in severity.
Once a patient is symptom-free and their neurological and cognitive testing returns to baseline levels, they may begin a graduated, return to play protocol. Zeeland requires that every athlete who sustains a concussion, regardless of origin, complete an approved Return To Activity Protocol (RTAP) under the direct supervision of an affiliated athletic trainer.
Post-Concussion Syndrome
The vast majority of concussions are found to resolve within 10-14 days after the onset of symptoms, however some cases can persist for several weeks or months. Once concussion symptoms extend past the 10-14 day acute period, they are no longer considered to be part of the initial injury and are instead categorized as post-concussion related.
Research is still developing in this area with experts divided on whether these unresolved symptoms are a result of structural damage and disrupted neuropathways or rather related to psychological factors, as the most common symptoms — headache, dizziness, and sleep problems — are similar to those often experienced by people diagnosed with depression, anxiety, or post-traumatic stress disorder (PTSD). Additionally, those with a history of depression, anxiety, or PTSD, as well as factors such as significant life stressors, a poor social support system, and lack of coping skills see higher frequencies of developing post-concussion symptom. Developing post-concussion symptoms does not, however, seem to be related to the severity of the initial injury.
Baseline Concussion Testing
Baseline neurocognitive testing, such as Concussion Vital Signs (CVS), has become standard practice to best provide a pre- and post-injury comparison of brain function. Tests like CVS are designed to be tools to guide return to physical and academic activities, however they are in no way a diagnostic test. "Passing" the CVS test after injury does not mean that the student-athlete did not sustain a concussion. It merely means that the injury did not appear to significantly affect neurocognitive functioning in the categories measured by the test.
It is a school policy that all high school student-athletes have a valid baseline CVS test prior to any extracurricular athletic participation. Baseline tests must be updated every two academic years, typically completed prior to a student's freshman and junior year. Testing is done at home, please contact your AT for more information.
Concussion Specialists
Most acute concussions can be managed by your school athletic trainer in conjunction with your primary-care physician, however, as discussed above, some cases do require more specialized evaluation and oversight. Specialty-trained physicians can perform targeted evaluations to identify specific deficits in individuals suffering from an acute concussion or post-concussion syndrome. These specialized individuals can best assess, treat, and coordinate care for the full spectrum of physical, cognitive, and emotional factors involved in concussion management.
Corewell Health Sports Concussion Clinic
References & Resources:
Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016
https://bjsm.bmj.com/content/51/11/838.long
Sports-Related Concussion in Children and Adolescents,
Pediatrics Sept. 2010 Vol. 126 Issue 3
http://pediatrics.aappublications.org/content/126/3/597
American Medical Society for Sports Medicine Position Statement: Concussion in Sports
http://journals.lww.com/cjsportsmed/Fulltext/2013/01000/American_Medical_Society_for_Sports_Medicine.1.aspx
Centers for Disease Control
http://www.cdc.gov/HeadsUp/index.html
The Knockout Project
http://theknockoutproject.org/?page_id=141

